Cardiovascular diseases (CVD) are a top concern for Medicaid Managed Care plans. A group of disorders of the heart and blood vessels, CVD is the leading cause of death in the U.S., costing $251 billion a year in direct medical costs. Medicaid case managers and care coordinators play a critical role in improving cardiovascular outcomes, yet managing these high-risk populations and their complex needs has historically been a challenge. Through collaborative care models and innovative engagement strategies, however, plans can close care gaps, reduce hospital readmissions, and enhance member well-being.
Addressing Cardiovascular Disease Among Medicaid Populations
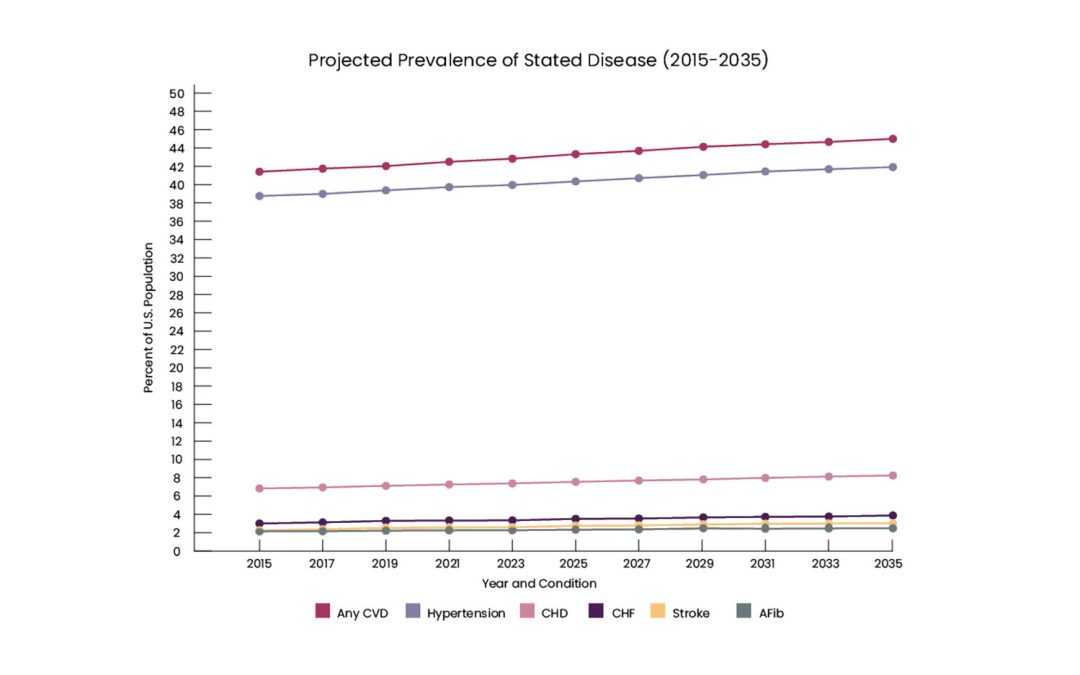
With rising rates of diabetes, obesity, cases of CVD are expected to surge in the coming years. By 2035, the number of those with CVD is projected to increase to 131.2 million—representing 45% or a staggering nearly half of the total U.S. population. of the total U.S. population.
(“Projected Prevalence of Stated Disease” page 7).
By 2035, the cost of CVD is expected to reach $1.1 trillion.
Disparities are also seen among these populations. CVD and its associated risk factors disproportionately affect many racial and ethnic groups, and account for nearly 40% of the disparity in life expectancy between black and white individuals. Heart failure, in particular, is associated with higher rates of healthcare utilization and hospital readmissions among Medicaid populations.
Research shows collaborative care models can improve care and result in 13% PMPM (per member per month) total health care cost savings, according to one study. With comprehensive strategies that include proactive, personalized care and the right technology, case managers can better support these high-risk patients, ensuring they receive the right care and support at the right time.
Here are 3 key areas for Medicaid case managers to focus on:
Take An Interdisciplinary Approach
According to a 2020 scientific statement, the American Heart Association stated that interdisciplinary care is necessary to achieve optimal population cardiovascular health. An interdisciplinary team approach combines multiple specialties and subspecialties including general cardiology, interventional cardiology, primary care, nursing, social work, as well as members and their caregivers. Engagement solutions can empower case managers to deliver an interdisciplinary approach for managing cardiovascular populations. With phone outreach and 2-way voice communication through Personal Emergency Response Systems (PERS), these solutions improve access and close care gaps by helping members:
- Identify primary and specialty care providers
- Schedule screenings and follow ups
- Adhere to prescribed medications
Invest In Digital Health Solutions
Nearly 90% of health plan executives say remote monitoring devices are effective in managing chronic illness, allowing for more personalized and proactive care plans, a 2024 survey found.
Remote Patient Monitoring (RPM) can help improve access to care, manage risk by monitoring blood pressure, for example, provide timely interventions, and drive patient engagement and treatment adherence.
Several systematic reviews and meta-analyses show that RPM can improve CVD care management, including identifying clinical events faster, reducing hospital readmissions and mortality rates, and improving quality of life. In fact, a 2024 study among patients with respiratory or cardiovascular diseases found after 6 months of using RPM, the average number of ED visits and hospitalizations decreased by 58%.
When paired with Remote Patient Monitoring (RPM), Personal Emergency Response Systems (PERS) empower care teams to track vitals, gain real-time data insights, and actively engage members in their care. Additionally, recognizing that movement is often the best medicine, newer PERS devices now feature a daily step-count function. This not only provides activity feedback to the user but also keeps caregivers and long-term care support coordinators informed. Even a small nudge—like wearing a PERS wristband—can encourage movement and help combat a sedentary lifestyle, making every step a step in the right direction.
Address Social Determinants of Health (SDoH)
Medicaid populations are more likely to have SDoH needs, unmet, non-medical needs that can drive between 80 and 90% of health outcomes. SDoH are linked to health disparities, inequities, and poor outcomes such as increased ED and hospital admissions.
The percentage of people with CVD who face food insecurity has more than doubled over the last 20 years.
Among members with cardiovascular conditions, factors such as food insecurity, health literacy, language barriers, and “super” social determinants of health such as digital access and digital skills can affect their ability to engage in their care and adhere to treatment.
To identify and address SDoH factors, close care gaps, and drive better cardiovascular outcomes, Medicaid managed care plans should consider engagement solutions that combine high-tech and high-touch approaches.
These solutions combine RPM and PERS devices with a dedicated team of wellness advocates who proactively engage with members to facilitate preventative care. Advocates conduct outreach to identify needs and connect members to resources such as local food banks. They also ensure devices and equipment are properly tested, and provide support when a low battery is detected or members need help using the technology, for example. Targeted engagement campaigns can ensure members schedule their vaccinations and complete health screenings. With this unique approach, members receive personalized, proactive care that leads to better outcomes and lower costs.
Improve Cardiovascular Outcomes With MedScope
Engagement is the key to closing cardiovascular care gaps and improving outcomes among Medicaid populations. MedScope is a leading provider of PERS and RPM solutions, allowing care managers to deliver proactive, patient-centric care. Our AI-powered solution combined with our highly empathetic wellness team connect and build trusted relationships with members to close care gaps and drive engagement. Ready to enhance cardiovascular care for Medicaid populations? Schedule a demo or contact us today.